Why your drugs don't work
There are drugs that come as tablets or capsules and can be kept at room temperature. Then there are drugs that patients will not usually handle—reagents used by diagnostic centres to conduct tests or intravenous drugs administered by medical professionals.
These are usually temperature-sensitive and need to be stored properly. There is no way for a patient to know if a diagnostic test is being done with denatured or date-expired medicines. A year-long investigation into the supply sector of intravenous drugs and reagents and diagnostic centres shows the public health disaster we are facing.
During a visit to the Bangladesh Medical Association building market last week, EM Surgicals was found to be storing antibiotic disks for diagnostic tests in a refrigerator set to 11 degree Celsius. This is way beyond the recommended temperature range in which such a product can be stored. This essentially means that the diagnostic tests done with these disks may not be accurate.
The market was busted in October last year by a Rapid Action Battalion (RAB) unit led by Magistrate Sarwoer Alam. Several shops were found selling expired insulin and reagents, namely Lotus Surgical, Midland, SA Surgical, Medifair, Bhuiya Surgicals, EM Surgicals and Atlanta Medica.
They were fined and given jail terms but the recent visit shows that EM Surgicals has gone back to their old ways.
A RAB unit raided two pharmaceutical distributors in Shyamoli on November 1 last year and found them selling large quantities of expired drugs and diagnostic reagents. None of the drugs or reagents were stored at their proper temperatures, thus effectively denaturing them; the warehouses kept no record of where and when they were manufactured. Magistrate Sarwoer Alam fined the distributors, LifeTech and VieTech a sum of BDT 18 lakh.
Officials found only two medium-sized refrigerators in the warehouses despite the large volume of temperature sensitive drugs they handle. This gave them adequate reason to believe LifeTech and VieTech have consistently sold expired products.
"All diagnostic tests done with products sold by these distributors are compromised because there is no guarantee Lifetech and Vietech had not supplied expired products," says Dr Mohammad Shahjahan, Assistant Director of the Directorate General of Health, who was present on spot.
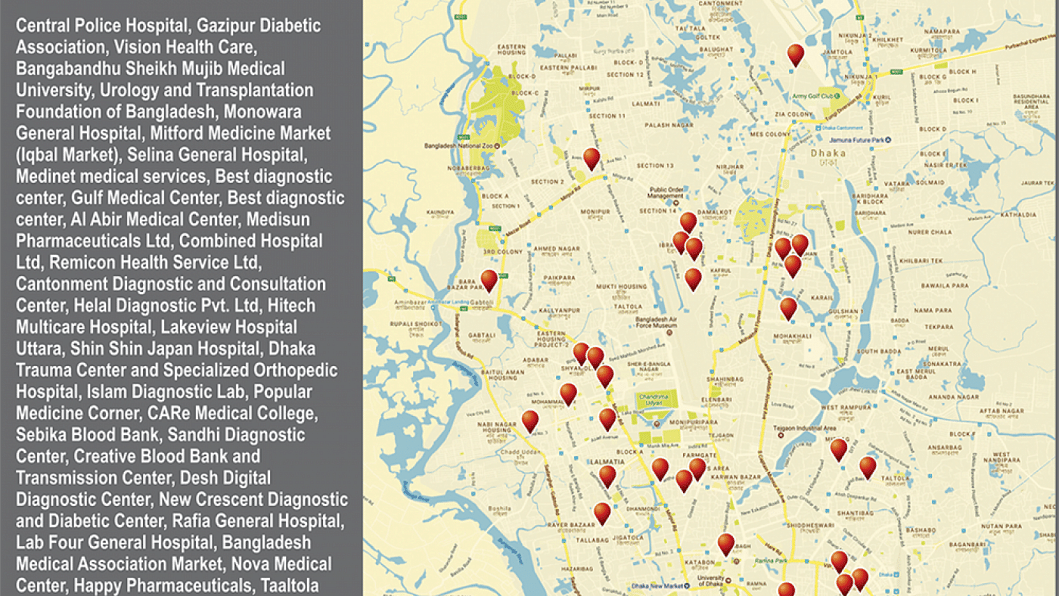
Of the many drugs seized by RAB, we chose three types of expired diagnostic test reagents—HbA1c (a blood sugar level test), SdA1c (a haemoglobin test), and hsCRP (a test for C-Reactive protein for assessing heart disease risk)—and examined sales invoices to find out which hospitals were regular customers.
It cannot be said for sure if they were all sold expired products because the distributors kept no documentation of their shipments, but it can be concluded that the diagnostic tests done with these products were compromised since Lifetech and Vietech did not have proper storage conditions. Noorjahan Hospital in Sylhet bought the highest number of units from these distributors—1200 units of hsCRP worth BDT 271,800. This means that 1200 diagnostic tests done at the hospital to gauge heart disease between November 2015 and June 2016 were compromised.
One of the largest hospitals in the city, and ironically enough, the hospital run by the law enforcers themselves, Central Police Hospital, was found to be a regular customer of Vietech. The distributor sold them BDT 195,000 worth of reagents between February and September. "We acquired our equipment from Vietech, so unfortunately we have purchased a lot of reagents from them too to fit the machines," says Dr Golam Quraishi, who heads the diagnostics department of the hospital. According to the Vietech sales invoices, the hospital has used 750 units of reagents.
According to the hospital's contract with Vietech, the distributors are supposed to bring in the drugs via a cold chain import process, states Quraishi. When Vietech delivers the drugs, they arrive in coolers, stored under the right temperatures, he says. "The packaging however is theirs. This is making me wonder whether they simply import in bulk, store under uncontrolled temperatures in their warehouses and then re-package it in coolers when someone wants to buy," he adds. Essentially he is wondering whether this is the scenario: Central Police Hospital requests a certain number of drugs, but the distributor brings in more at once, to avoid the costs of making multiple air-freights. Then the distributor breaks open the cooler, re-packages the number needed by the hospital and stores the rest in a warehouse without temperature control. The next time the hospital wants some more reagents again, they simply take them off the shelves, put them in a cooler and deliver.
During a conversation with the Chief Operating Officer of Vietech Mohammed, Mobarok Hossain, he claimed that they have since tried to maintain quality. "Central Police Hospital also made an inquiry after the raid," says Hossain, "It would also be helpful for us if the government authorities gave us recommendations on how to do our business." Lifetech's Chief Executive Officer Mohammed Ashaduzzaman could not be reached over the phone last week.
The two drug distributors jointly sold a further BDT 337,200 worth of these reagents to Gazipur Diabetic Samity, Ibn Sina Sylhet, Vision Health Care, Unitech, Urology and Transplantation Foundation of Bangladesh and Monowara General Hospital during different periods last year. In effect, more than a 1000 tests done for blood sugar, haemoglobin and heart disease in these hospitals and diagnostic centres last year can be said to have been compromised. Lifetech also supplied temperature-sensitive products to other hospitals and diagnostic centres like Bangabandhu Sheikh Mujib Medical University (BSMMU), Square Hospital and Ibn Sina Hospital, but they did not purchase the same kind of drugs that were confiscated by RAB during the raid. It must be reiterated, however, that the mobile court magistrate deemed the storage capacity of the distributors as inadequate. If indeed these well-known hospitals were sold denatured reagents, then they were simply unwitting victims.
"All our reagents are directly imported from abroad and we only buy a small quantity locally," says Dr Anowarul Hossain, the Head of Diagnostics of Square Hospital. This corresponds to the invoice – they only made purchases worth BDT 53,000—a lesser amount compared to the other hospitals.
That most doctors invariably experience denatured products can be attested by Dr Shohael Mahmud Arafat, Professor at BSMMU. "We make sure that our patients do tests at trusted laboratories known among physicians for using good quality drugs," he says.

What is a cold chain (supply chain) and how do drug supply chains break?
To answer this question, we interview Anand Shetty, the Managing Director of Novo Nordisk. To demonstrate an example of a cold chain model, Shetty describes how they import insulin. Insulin is one of the many life-saving drugs that can get denatured if not stored in proper temperatures.
"When we import our insulin from Europe, with each box is attached a thermostat that logs the temperature during transportation from the point of exit to the final destination," informs Shetty.
When the shipment arrives to the warehouse in Bangladesh, quality control personnel check the temperature log of each box, and report it back to the exporting country, describes Shetty.
"The shipment is authorised for distribution only after the headquarters have confirmed that the temperature has remained consistent," he continues. If there is deviation from the given temperature range at any point during transportation such that the insulin's quality may be jeopardised, the shipment is destroyed. "The drug-carrying coolers are sent to the many branches of our distribution centres in authorised cold chain vans that maintain a temperature of 2–8 degree Celsius," adds Shetty. The distribution centres than deliver the coolers to pharmacies, who are ideally supposed to take them out and store them in proper conditions until purchased.
A cold chain breaks when one actor does not maintain proper storage temperatures. This can happen at the supplier's warehouse, or it can happen in pharmacy retailers. But it all boils down to this: Is the lack of a regular refrigerator that can maintain temperatures up to -20 degree Celsius causing a public health disaster?
"We have no control over what happens after the drugs reach the pharmacy," says Shetty. "We raise awareness among them about proper storage, but we obviously cannot monitor them."
One would be hard-pressed to find out exactly who can monitor them. There are over a hundred thousand pharmacies according to the Directorate General of Drug Administration (DGDA). The DGDA inspected 136 of them last month. The highest-ever number of inspections was in May 2015, when they hit 960 spots. This means that the DGDA can only effectively inspect an insignificant fraction of all the pharmacies in the country. The existence of mobile courts also hangs in the balance at the moment. Having said that, it is imperative to question whether pharmacy inspections are even the right method of ensuring quality.
Stakeholders agree that having licensed registered pharmacists is one way for pharmacies to have integrity and medical understanding about how to store drugs. But compared to the hundreds of thousands of pharmacies, there are only 11,426 licensed degree-holding (grade-A) pharmacists in the country. A 2015 nationwide study done by WHO found that almost half of the pharmacies they sampled did not have a licensed pharmacist. Of those who did, the overwhelming majority only had a certificate course to boast of.
"Doing inspections cannot be the only way of ensuring pharmaceutical quality. We need to raise awareness on the risks of not having quality drugs. This requires a joint commitment from medical associations, pharmaceutical associations and all concerned departments," comments Sarwoer Alam, the Executive Magistrate of RAB who was in charge of many of the raids mentioned in the story. He has led mobile courts on hundreds of pharmaceutical raids during his term.
How widespread is the problem?
Last year in November, the RAB went into the Mitford Medicine Market and confiscated cartons and cartons of intravenous drugs all of which needed to be stored under 8 degree Celsius, but were being kept at room temperature—which in Dhaka can mean a sweltering 40 degree Celsius. These included very expensive drugs used to tackle clotting disorders: Baxter Immunate 500 IU which is priced at USD 300 according to drug database ODDB.org, and Xyntha Antihemophilic, costing USD 407. Also confiscated were immunosuppressants (Sandimmun), human albumin, vasodilators and hormones used for breast cancer and prostate cancer (zoladex goserelin). Boxes of date expired oral medicines, like cyclogest, feroglobin, janumet, imuran, amantrel and tenoret, were also seized.
On another occasion last December, the mobile court busted one of Kafrul's biggest hospitals, Hitech Multicare Ltd, for using expired tumour markers to test for cancers of the stomach, colon, prostate, liver, etc. The marker kits, which are used to detect alpha-feroprotein and carcinoembryoinc antigen in blood, can each be used to perform a 100 diagnostic tests. The mobile courts found two such kits in use, meaning the cancer diagnoses of 200 patients were jeopardised.
The hospital was also stocking date-expired drugs in their pharmacy, all of which were expired by several months to a year. The confiscated stock included both oral and in-vitro drugs and antibiotics. They found vials of a drug called amiodarone used to treat arrhythmia of the heart, and an in-vitro solution for tackling inflammation called triamcinolone acetonide.
Other renowned hospitals and diagnostic centres busted for using or selling denatured reagents include Dhaka Trauma Centre and Specialised Orthopaedic Hospital and Care Medical Centre in Shyamoli.
"This can be called a national disaster," says Dr Shohael Arafat, "There have been times when a patient has been given insulin but it has no effect on the blood sugar, or administering albumin does not change the protein levels."
Dr Quazi Rakibul Islam, the General Secretary of Doctors for Health and Environment, thinks that there needs to be a large-scale consultation with doctors of different disciplines to record their experiences.
This investigation is only a preliminary step. What must follow is a commitment from the authorities to tackle the situation.
Supported by Brown Institute of Media Innovation
Syed bin Amir contributed to this story.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 






Comments