Cervical cancer prevention
Cervical cancer is the fourth most common cancer among women globally, with an estimated 604 000 new cases and 342 000 deaths in 2020. About 90% of the new cases and deaths worldwide in 2020 occurred in low- and middle-income countries. The Human Papillomavirus (HPV) that causes cervical cancer is mainly transmitted through sexual contact and most people are infected with HPV shortly after the onset of sexual activity. More than 90% of them clear the infection eventually.
Vaccination against HPV and screening and treatment of pre-cancer lesions are cost-effective ways to prevent cervical cancer. Cervical cancer can be cured if diagnosed at an early stage and treated promptly. Comprehensive cervical cancer control includes primary prevention (vaccination against HPV), secondary prevention (screening and treatment of pre-cancerous lesions), tertiary prevention (diagnosis and treatment of invasive cervical cancer) and palliative care.
Cervical cancer prevention should encompass a multidisciplinary, including community education, social mobilisation, vaccination, screening, treatment, and palliative care.
It is important for both girls and boys to be offered appropriate health information and warnings about tobacco use, as well as sex education tailored to their age and culture. Additionally, promoting and providing access to condoms for those engaged in sexual activity can help. Male circumcision can also reduce STI risk and offer health benefits. Healthcare professionals and personal and cultural values should guide these decisions.
HPV vaccination
There are currently four vaccines that have been prequalified by the World Health Organisation (WHO). To prevent cervical cancer WHO recommends vaccinating girls aged 9 to 14 years.
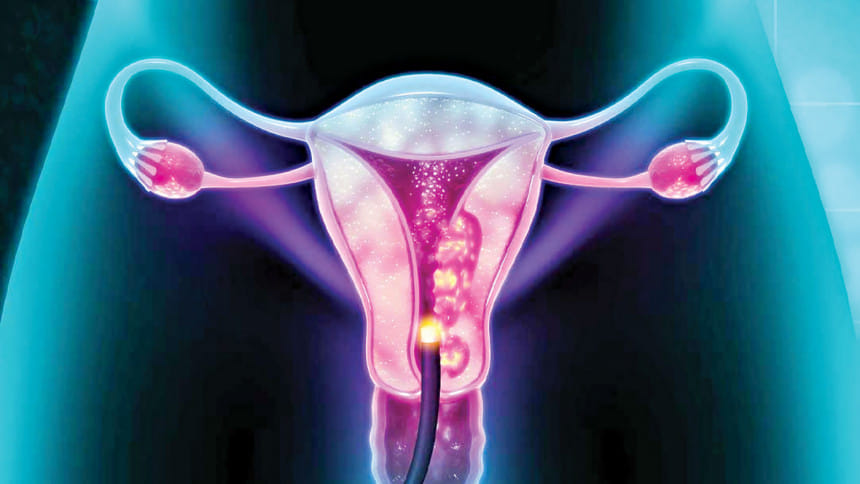
Screening and treatment of cervical pre-cancer lesions
Cervical cancer screening involves testing for HPV infection.When screening detects an HPV infection or pre-cancerous lesions, these can easily be treated and cancer can be avoided. Screening can also detect cancer at an early stage where treatment has a high potential for cure.
Screening should start at 30 years of age in the general population of women, with regular screening with a validated HPV test every 5 to 10 years, and at 25 years of age for women living with HIV. Women living with HIV also need to be screened every 3 to 5 years.
A woman with symptoms of suspicion for cervical cancer must be referred to an appropriate facility for further evaluation, diagnosis and treatment.
WHO has developed guidance and tools on how to prevent and control cervical cancer through vaccination, screening and treatment, management of invasive cancer. WHO works with countries and partners to develop and implement comprehensive programmes in line with the global strategy.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments