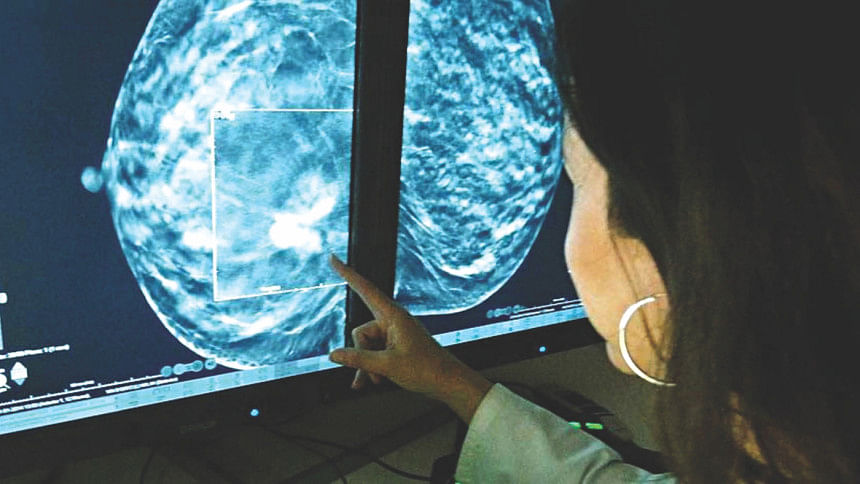
Precision in the treatment of breast cancer
Worldwide, breast cancer is the most-common invasive cancer in women. It affects about 12% of women worldwide. Breast cancer comprises 22.9% of invasive cancers in women and 16% of all female cancers.
Dr Radhika Lakshmanan, a Senior Consultant General Surgeon, who has special interest in breast cancer and reconstructive surgery working at the Farrer Park Hospital, Singapore recently shared her views with Star Health on breast cancer.
Since breast cancer is very common and the specialty has already drawn the attention, almost all the countries have some capacity to deal with the problem. She was asked how Singapore was different in treating breast cancer.
She informed that there is a certain protocol that is maintained in Singapore which makes significant differences in the treatment. For example, minimally invasive surgery of lymph nodes or the sentinel lymph node biopsy.
A sentinel lymph node is defined as the first lymph node to which cancer cells are most likely to spread from a primary tumor. Sometimes, there can be more than one sentinel lymph node. A sentinel lymph node biopsy (SLNB) is a procedure in which the sentinel lymph node is identified, removed, and examined to determine whether cancer cells are present.
This is not done in most of the countries in Asia. Even in early breast cancer surgery, all the lymph nodes are removed which causes lots of complications like swelling of the arm. It hampers the lifestyle of the patient to a great extent.
Another example is the removal of the whole breast. In most of the countries, the whole breast is removed. But in Singapore, they give neoadjuvant chemotherapy for breast cancer. It refers to medicines that are administered before surgery for the treatment of breast cancer. Doctors may recommend neoadjuvant chemotherapy due to the size of the tumor, since the drugs may shrink the tumor and give more surgical options. It helps in downstaging of the tumour.
The third reason Dr Radhika pointed out is the availability of latest drugs in Singapore. Patients get the most advanced medicine for the treatment. Alongside, they are provided treatment with the use of latest cutting-edge technology for diagnosis and prognosis. For example, an accurate tissue analysis (e.g. genetic analysis of tissue) can alter the whole treatment guideline.
Oncotype DX test is a genomic test that analyses the activity of a group of genes that can affect how a cancer is likely to behave and respond to treatment. The Oncotype DX is used in two ways:
1) to help doctors figure out a woman's risk of early-stage, estrogen-receptor-positive breast cancer coming back (recurrence), as well as how likely she is to benefit from chemotherapy after breast cancer surgery.
2) to help doctors figure out a woman's risk of Ductal Carcinoma in situ (DCIS) coming back (recurrence) and/or the risk of a new invasive cancer developing in the same breast, as well as how likely she is to benefit from radiation therapy after DCIS surgery.
Of all the breast cancer genomic tests, the Oncotype DX test has the strongest research behind it. The results of the Oncotype DX test, combined with other features of the cancer, can help the patients make a more informed decision about whether or not to have chemotherapy to treat early-stage, hormone-receptor-positive breast cancer or radiation therapy to treat DCIS.
An advocate of breast cancer awareness, Dr Radhika also explained how a partial breast surgery followed by oncoplastic and reconstructive surgery helps a patient in breast cancer management.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments