The malaise of antibiotic overuse
Overusing antibiotics for illnesses that do not require such medication has been on the rise in Bangladesh, indicates recent icddr,b studies.
A recent study that examined the use of antibiotics by children under two years of age in Dhaka has shown that each child has taken over 10 antibiotic courses per year on average – an alarmingly high rate compared to global standards.
In the US, children less than two take 0.9 to 1.7 courses per year, notes the study conducted on eight countries in the global South (Bangladesh, Brazil, India, Nepal, Pakistan, Peru, South Africa and Tanzania). The study found that children in these countries have taken almost five courses (4.9) a year on average primarily to treat diarrhoeal and respiratory illnesses.
"It is a matter of worry that antibiotics are often prescribed without knowing the consequences it might lead to," says Dr Tahmeed Ahmed, Senior Director of nutrition and clinical services at icddr,b and a co-author of the study published in the Bulletin of the World Health Organization (WHO).
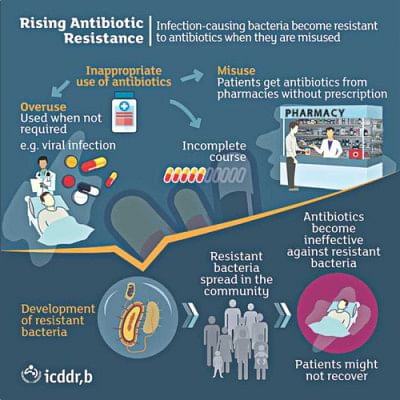
It is now widely known that antibiotic misuse causes them to become ineffective because the infection-causing bacteria become resistant to these drugs – a phenomenon known as antibiotic resistance. Rising antimicrobial resistance (AMR) of microorganisms such as bacteria, virus, fungus and parasites is now a global concern worldwide.
Since the ill-effects of antibiotic misuse are less known, the WHO in its global action plan on AMR has advised improving awareness and understanding of antimicrobial resistance through effective communication, education and training.
"We frequently see in the community that patients bypass doctors and directly purchase antibiotics from pharmacies where it is widely available without prescription," adds Dr Mustafa Mahfuz, Deputy Project Coordinator at icddr,b and a co-author of the study.
In order to ascertain antibiotic consumption by consumers, the WHO has laid out surveillance guidelines which can be adopted at the national levels. This can help reduce over-the-counter sale of antibiotics.
When it comes to children, the WHO also has specific Integrated Management of Childhood Illness (IMCI) guidelines that prescribe antibiotics for certain health conditions, not all. "Using antibiotics in cases where it is not required can apparently cure the children but causes lifelong harm that cannot be reverted," adds Dr Mahfuz.
Poor enforcement of laws to limit access to antibiotics is one of the reasons that their abuse persists in countries like Bangladesh and Pakistan. The study also found that those who can afford these drugs have a higher tendency to overuse them.
The eight-country study, called the Etiology, Risk Factors and Interactions of Enteric Infections and Malnutrition and the Consequences for Child Health and Development Project (MAL-ED), is carried out as a collaborative project supported by the Bill & Melinda Gates Foundation, the Foundation for the NIH and the National Institutes of Health/Fogarty International Center.
Another recent icddr,b study has found rising antibiotic resistance to bacterial pathogens which cause bloodstream infections – a condition when bacterial infection elsewhere in the body enters the bloodstream.
Dr Dilruba Ahmed, head of clinical microbiology and immunology at icddr,b, has studied over 100,000 blood samples from a period of over ten years and tested them for the presence of pathogens and the incidence of antibiotic resistance in these pathogens. A high percentage of these bloodstream pathogens have acquired multidrug resistance (i.e. they are resistant to a number of antibiotics), according to the findings published in BMC journal Antimicrobial Resistance & Infection Control.
"The problem is that even if you stop using these antibiotics, the bacterial pathogens are not going to go back to their earlier state. They remain resistant to certain drugs which will hardly work for those patients," says Dr Ahmed.
She expects that the study will help healthcare professionals including private practitioners to make informed decisions while prescribing antibiotics. "A nationwide guideline for antibiotic prescription and its enforcement should be really helpful," she adds.
The study was funded by core donors including Bangladesh Government, Global Affairs Canada (GAC), Swedish International Development Cooperation Agency (Sida) and the Department for International Development (UK Aid).
"Bangladesh is yet to bridge the knowledge gap regarding antimicrobial resistance," says Dr Mohammad Aminul Islam, associate scientist at icddr,b and a member of the WHO Advisory Group on Integrated Surveillance of Antimicrobial Resistance (WHO AGISAR). He is currently leading a number of studies at icddr,b to generate knowledge on AMR, considering it a One Health problem.
The WHO developed a global action plan and a manual for developing national action plans to address AMR in early 2016. It suggests country-specific actions to optimise the use of antimicrobial medicines in human and animal health.
"Bangladesh needs an improved surveillance of antibiotic resistance, regulation of the appropriate use of quality medicines, and education about the consequences of overuse," says Dr Amin.
Alongside ongoing research activities at icddr,b, tackling AMR in Bangladesh will also require that relevant policymaking bodies raise awareness around this issue and implement policies to regulate access to antibiotics in order to stop their misuse and overuse.
The writer is a communication specialist at icddr,b.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments