Managing angina without surgery
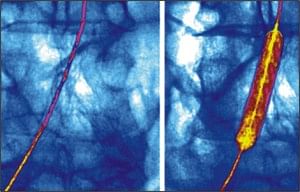
Drug therapy may be as effective as angioplasty, above, or other invasive interventions used to manage angina, new research suggests.
There are several modern invasive tools cardiologists are using to treat angina (chest pain) including angioplasty (blowing up balloons to expand the artery at sites of block), stenting (insertion of cylindrical wire mesh tube prop open the blocked artery) and bypass surgery (increasingly through very small incisions). But drug therapy may be just as effective to restore blood flow as invasive surgery for stable angina, a new analysis published in The New England Journal of Medicine suggests.
Angina is chest pain or discomfort that occurs when an area of heart muscle does not get enough oxygen-rich blood. It is often a warning sign of an impending heart attack. If a coronary artery (arteries which supply blood to heart) becomes blocked, either by fatty material or a blood clot, then part of the heart muscle is starved of oxygen. Due to blockages in the heart's arteries, affected person may feel like pressure or squeezing in chest. The pain also may occur in shoulders, arms, neck, jaw, or back. It can feel like indigestion.
Invasive treatments are found to relieve symptoms decisively in most patients. They actually prevent impending heart attacks and deaths only in special circumstances notably, when patients are treated within a few hours of an acute heart attack.
On the other hand, simple and cost-effective drug treatment can give patients the same advantage. Cardiologists now have several effective classes of drugs that have the estimable ability to reduce the heart's workload, improve blood flow by dilating arteries, and increasingly target the diseased artery itself.
Often, patients and their physicians confront when to turn to the invasive strategies that have long been a mainstay of angina management. A recent analysis of data from pivotal clinical trial called COURAGE provides some important new insights.
In this study, over 2,000 patients with stable angina were randomised into groups receiving aggressive drug therapy with or without additional angioplasty and stenting. The primary results, published in 2007, showed no additional benefit to invasive treatments with regard to heart attack or deaths in the group during 4.6 years of follow-up.
The new data, published last month in The New England Journal of Medicine, revealed whether adding invasive treatment to intense medical treatment reduced the frequency of angina and improved quality of life and well-being in these patients.
Shortly after treatment, the patients who had invasive revascularisation reported slightly less angina and slightly better quality of life. But by the end of the 4.6 years of follow-up, the patients who did not receive invasive treatments were faring as well as those who did (although about one-fifth of those originally treated without surgery ultimately required mechanical revascularisation).
From the expert analysis on the study we can learn two important lessons. First, starting aggressive therapy, be it with drugs or drugs plus surgical revascularisation, improved symptoms and quality of life in both groups promptly in the case of surgical revascularisation, but rapidly even for drug therapy alone. This is extremely good news for patients with angina: modern therapy is quick, effective and results in an excellent quality of life in most individuals.
The surprising and progressive benefit of non-invasive therapy may come about because some of the newer drugs favorably alter the biology of the artery and plaque (fatty deposits). Several drugs notably statins and agents that interrupt the action of the hormone angiotensin (causes blood vessels to constrict, and drives blood pressure up) are quite effective. Statins lower bad cholesterol (LDL), one of the drivers of atherosclerosis, and also appear to calm inflammation in the plaque independent of effects on LDL. Blocking angiotensin action may also provide a benefit to arterial health beyond just lowering blood pressure.
The second message: we do not need to rush into surgery as a first step in people with stable angina. Along with drug therapy lifestyle changes like quitting cigarettes, losing excess body fat, switching to a low fat diet and taking regular exercise (such as walking every day) can significantly improve the condition. They can help dampen the need of surgery. Invasive strategies are only needed if these non-invasive measures are proved to be ineffective. These new data, in the context of many other studies, will help cardiologists to take a staged approach to the management of stable angina with confidence that this implication does not jeopardise longevity or increase risk of heart attacks.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments