|
Health
The
Truth About
Pneumonia
Farhat Mustafa
 What is pneumonia?
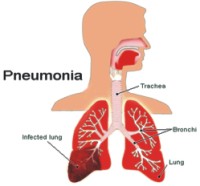
Pneumonia is an infection of one or both lungs which is usually caused by bacteria, viruses, or fungi. Prior to the discovery of antibiotics, one-third of all people who developed pneumonia subsequently died from the infection.
How do people "catch pneumonia"?
Some cases of pneumonia are contracted by breathing in small droplets that contain the organisms that can cause pneumonia. These droplets get into the air when a person infected with these germs coughs or sneezes. In other cases, pneumonia is caused when bacteria or viruses that are normally present in the mouth, throat, or nose inadvertently enter the lung. During sleep, it is quite common for people to aspirate secretions from the mouth, throat, or nose. Normally, the body's reflex response (coughing back up the secretions) and immune system will prevent the aspirated organisms from causing pneumonia. However, if a person is in a weakened condition from another illness, a severe pneumonia can develop. People with recent viral infections, lung disease, heart disease, and swallowing problems, as well as alcoholics, drug users, and those who have suffered a stroke or seizure are at higher risk for developing pneumonia than the general population.
Once organisms enter the lungs, they usually settle in the air sacs of the lung where they rapidly grow in number. This area of the lung then becomes filled with fluid and pus as the body attempts to fight off the infection.
What are pneumonia symptoms?
Most people who develop pneumonia initially have symptoms of a cold which are then followed by a high fever (sometimes as high as 104 degrees Fahrenheit), shaking chills, and a cough with sputum production. The sputum is usually discoloured and sometimes bloody. Patients may become short of breath. Chest pain may develop if the outer aspects of the lung are involved. This pain is usually sharp and worsens when taking a deep breath, known as pleuritic pain.
In other cases of pneumonia, there can be a slow onset of symptoms. A worsening cough, headaches, and muscle aches may be the only symptoms. In some people with pneumonia, coughing is not a major symptom because the infection is located in areas of the lung away from the larger airways. At times, the individual's skin colour may change and become dusky or purplish (a condition known as "cyanosis") due to their blood being poorly oxygenated.
Children and babies who develop pneumonia often do not have any specific signs of a chest infection, but develop a fever, appear quite ill, and can become lethargic. Elderly people may also have few symptoms with pneumonia.
How Pneumonia is Diagnosed
* Tuberculosis Skin Test (PPD Skin Test) - The tuberculosis skin test (also known as the tuberculin or PPD test) determines whether a person has developed an immune response to the bacterium that causes tuberculosis (TB).
* Chest X-ray - A chest x-ray is a radiology test that involves exposing the chest briefly to radiation to produce an image of the chest and the internal organs of the chest. Chest x-ray can be used to define abnormalities of the lungs such as excessive fluid, pneumonia, bronchitis, asthma, cysts, and cancers.
* Bronchoscopy -, a procedure used to view a patient's lung, airways, voice box, vocal cord, trachea, and many branches of bronchi. There are two types of bronchoscopes, flexible fiberoptic and rigid.
Pneumonia may be suspected when the doctor examines the patient and hears coarse breathing or crackling sounds when listening to a portion of the chest with a stethoscope. There may be wheezing, or the sounds of breathing may be faint in a particular area of the chest. A chest x-ray is usually ordered to confirm the diagnosis of pneumonia.
Sputum samples can be collected and examined under the microscope. If the pneumonia is caused by bacteria or fungi, they can often be detected by this examination. It is important to understand that the sputum specimen must contain little saliva from the mouth and be delivered to the laboratory fairly quickly. Otherwise, overgrowth of noninfecting bacteria may predominate.
A blood test that measures white blood cell count (WBC) may be performed. An individual's white blood cell count can often give a hint as to the severity of the pneumonia and whether it is caused by bacteria or a virus.
Bronchoscopy is a procedure in which a thin, flexible, lighted viewing tube is inserted into the nose or mouth after a local anesthetic is administered. The breathing passages can then be directly examined by the doctor, and specimens from the infected part of the lung can be obtained.
Sometimes, fluid collects in the pleural space around the lung as a result of the inflammation from pneumonia. This fluid is called a pleural effusion. If the amount of this fluid that develops is large enough, it can be removed by inserting a needle into the chest cavity and withdrawing the fluid with a syringe in a procedure called a thoracentesis. In some cases, this fluid can become severely inflamed (parapneumonia effusion) or infected (empyema) and may need to be removed by more aggressive surgical procedures.
What causes pneumonia?
The most common cause of a bacterial pneumonia is Streptococcus pneumoniae. In this form of pneumonia, there is usually an abrupt onset of the illness with shaking chills, fever, and production of a rust-coloured sputum. The infection spreads into the blood in 20-30% of cases, and if this occurs, 20-30% of these patients die. A vaccine (Pneumovax) is available against S. pneumoniae and is recommended for the elderly, infants, people who have diabetes, chronic heart, lung, or kidney disease, those with alcoholism, cigarette smokers, and in those persons who have had their spleen removed.
Antibiotics often used in the treatment of this pneumonia include penicillin, amoxicillin and clavulanic acid (Augmentin, Augmentin XR), and macrolide antibiotics including erythromycin, azithromycin (Zithromax, Zmax), and clarithromycin (Biaxin).
Hemophilus influenza is a bacterium that often causes pneumonia in people suffering from chronic obstructive pulmonary disease (COPD) or alcoholism. Useful antibiotics in this case are the second- and third-generation cephalosporins, amoxicillin and clavulanic acid, fluoroquinolones (levofloxacin [Levaquin]), moxifloxacin-oral (Avelox), gatifloxacin-oral (Tequin), and sulfamethoxazole and trimethoprim (Bactrim, Septra).
Mycoplasma pneumonia is often a slowly developing infection. Symptoms include fever, chills, muscle aches, diarrhoea, and rash. This bacterium is the principal cause of many pneumonias in the summer and fall months and is often referred to as "atypical pneumonia." Macrolides (erythromycin, clarithromycin, azithromycin, and fluoroquinolones) are antibiotics commonly prescribed to treat Mycoplasma pneumonia.
Legionnaire's disease is caused by the bacterium Legionella pneumoniae and is most often found in contaminated water supplies and air conditioners. It is a potentially fatal infection if not accurately diagnosed. Pneumonia is part of the overall infection, and symptoms include high fever, a relatively slow heart rate, diarrhoea, nausea, vomiting, and chest pain. Older men, smokers, and people whose immune systems are suppressed are at higher risk of developing Legionnaire's disease. Fluoroquinolones are the treatment of choice in this infection.
Viral pneumonias do not typically respond to antibiotic treatment. These pneumonias usually resolve over time with the body's immune system fighting off the infection. It is important to make sure that a bacterial pneumonia does not secondarily develop. If it does, then the bacterial pneumonia is treated with appropriate antibiotics.
Major concerns have developed in the medical community regarding the overuse of antibiotics. Viruses rather than bacteria cause most sore throats and upper respiratory infections. Though antibiotics are ineffective against viruses, they are often prescribed. This excessive use has resulted in a variety of bacteria that have become resistant to many antibiotics. These resistant organisms are commonly seen in hospitals and nursing homes. In fact, physicians must consider the location when prescribing antibiotics (community-acquired pneumonia, or CAP, versus hospital-acquired pneumonia, or HAP).
Source: www.MedicineNet.com Copyright
(R) thedailystar.net 2007 |
